Elizabeth Nethery, University of British Columbia; Amanda Black, L’Université d’Ottawa/University of Ottawa; Amanda K Downey, McMaster University; Laura Schummers, University of British Columbia, and Wendy V. Norman, University of British Columbia
Why should women in British Columbia, Manitoba, Prince Edward Island and the Yukon have access to free contraception while the rest of Canadians do not? Our new research, published in the British Medical Journal and JAMA Pediatrics, underscores the urgent need for universal prescription contraception coverage nationwide. Spoiler alert: cost matters.
When B.C. launched universal coverage for prescription contraception in April 2023, more people used contraceptives, and importantly, more chose the most effective methods. When Ontario introduced universal coverage for those younger than age 25 in January 2017, we found a similar jump in the most effective contraceptive methods.
In October 2024, the National Pharmacare Act received royal assent, establishing a framework for a national, universal, single-payer pharmacare program, beginning with free access to contraception and diabetes medications. Now, almost a year later, only four provinces and territories (B.C., Manitoba, P.E.I. and the Yukon) have bilateral agreements to implement this legislation on the ground.
On Sept. 10, Prime Minister Mark Carney said the federal government is “committed to signing pharmacare deals with all provinces and territories.” This is welcome news given previous statements in July by Health Minister Marjorie Michel indicating wavering commitment or that “all options are on the table” for implementing Bill C-64 nationally.
Why affordable birth control is essential
As reproductive health policy researchers (including two health-care providers), we know that universal coverage for contraception is essential to uphold reproductive population health and to achieve gender equity in Canada. We have recently published evidence demonstrating the effect of universal contraception funding policies on contraception use, which reaffirm how critical this policy is in the Canadian context.
Everyone in Canada, regardless of income or postal code, deserves access to the contraception that is right for them, without cost standing in the way. As former Federal Health Minister Mark Holland stated when announcing national pharmacare on Feb. 29, 2024: “Waking up in a country where every single woman has access to the contraception she needs to control her future is an absolutely critical part of having a just society.” He added: “This is about health equity.”
When women can’t afford contraception, the risk of unplanned pregnancy increases. When contraception is accessible without financial or logistical barriers, women are more likely to plan pregnancies around their health, education, career and family goals. This benefits not only the individual but also children, families and society overall by improving gender equity in education and workforce participation, reducing poverty and supporting better health outcomes.
Beyond this, free contraception is a cost-effective policy, expected to save our health systems money in the long term by reducing health-care costs linked with unplanned pregnancies.
Private and public drug plans
Some critics argue that many Canadians already have drug insurance and plans that cover contraceptive costs. But that doesn’t tell the whole story.
Most private and public plans do not cover 100 per cent of prescription drug costs. Deductibles and co-pays leave patients paying at least a portion out-of-pocket, and some private plans exclude contraception altogether. The most effective contraceptives (intrauterine devices (IUDs) and subdermal implants) can cost up to $450 up front, even with coverage.
Many young people or those working in seasonal or temporary jobs don’t have drug insurance at all. Others choose to pay out-of-pocket to avoid having birth control charges show up on a shared plan with a partner, spouse or parent — to preserve privacy. That is why first-dollar, universal coverage for contraception — as outlined in federal pharmacare — is essential. It guarantees access free from financial strain, coercion, loss of privacy or compromise.
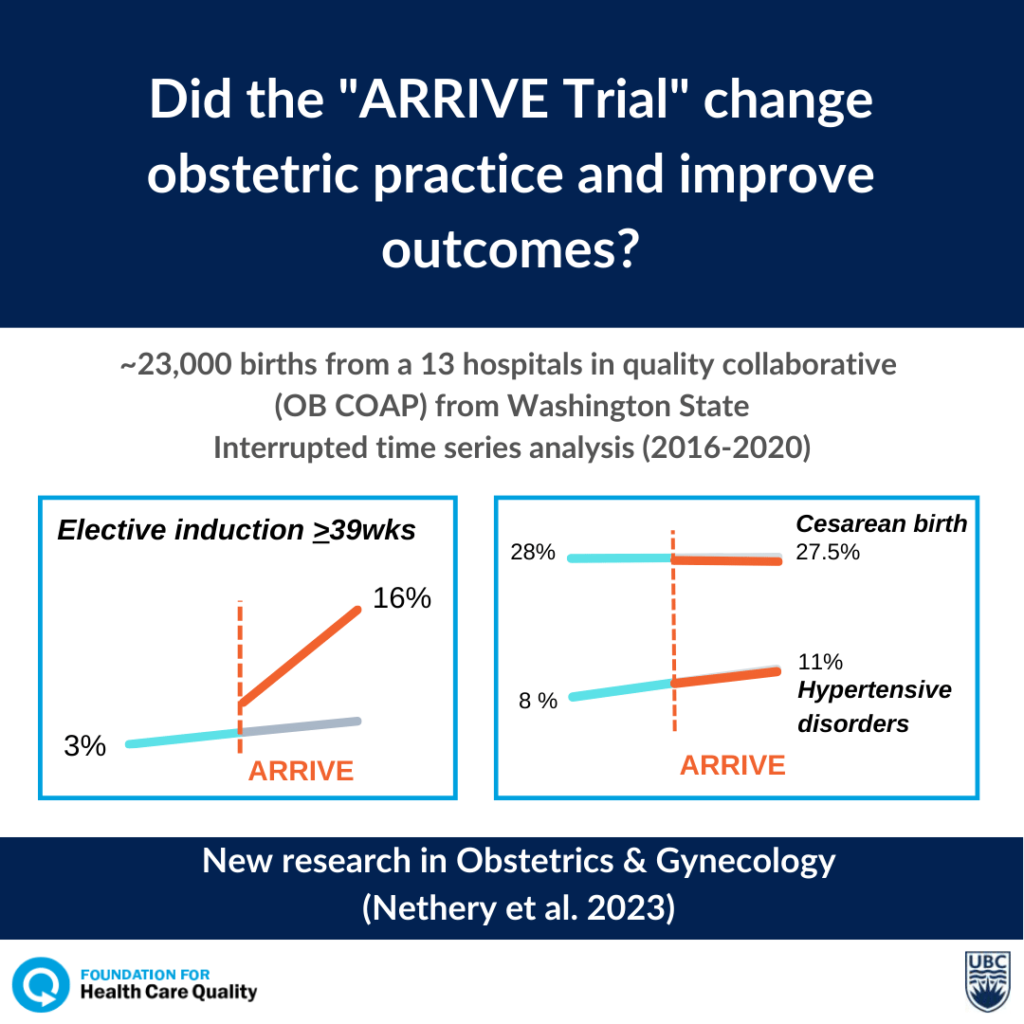
If Canada’s pre-existing mix of public and private insurance provided sufficient access to contraception, we would have seen little or no change when contraception became free in B.C. But we did see change. Our research showed a 49 per cent increase in the use of the most effective contraceptive methods when they were available at no cost.
Clear evidence for pharmacare
This provides clear evidence that cost has been a barrier for individuals in B.C. and highlights a critical point: without universal coverage, many Canadians simply cannot afford their preferred method of birth control. When costs are taken out of the equation, more people choose the most effective contraception methods.
Similarly, when Ontario provided universal prescription coverage for youth 24 years old or younger in 2018, we found that prescriptions for IUDs and oral contraceptive pills jumped, with the greatest increases for those in low-income areas.
When this coverage was revised to exclude those with private insurance, use declined. This shows us that private insurance is inadequate to cover gaps in contraception needs, especially for youth.
All Canadians seeking to manage their reproductive futures deserve equitable access to safe, effective and affordable contraception. Our new findings show just how strongly cost influences these choices.
The federal government has promised to implement national pharmacare, starting with contraception (and diabetes medication). On Sept. 2, Michel said “we are tracking those [agreements] that have already been done to see how it works.”
The evidence is now available and is clear: pharmacare works. Our analysis of B.C.’s policy shows the clear public health benefits that could result from expanding pharmacare and making no-cost contraception a reality for all Canadians. Further, our analysis of Ontario’s experience show that a watered-down version of pharmacare policy (like Ontario’s policy for youth since 2019) does not suffice.
All Canadians, regardless of where they live, deserve access to the contraception that they need to control and plan their reproductive health futures. Now is the time to implement universal, first-payer coverage for contraception for all Canadians.
Elizabeth Nethery, Postdoctoral research fellow, University of British Columbia; Amanda Black, Professor of Obstetrics and Gynecology, L’Université d’Ottawa/University of Ottawa; Amanda K Downey, PhD Candidate, Health Research Methodology, McMaster University; Laura Schummers, Assistant Professor, University of British Columbia, and Wendy V. Norman, Professor and Canada Research Chair, University of British Columbia
This article is republished from The Conversation under a Creative Commons license. Read the original article.